Dr.’s Culligan and Goldberg are donating all proceeds from the sales of this textbook to The American Urogynecologic Society Foundation.
Publications by Dr. Culligan
ALL OF THESE PUBLICATIONS ARE UNDER COPYRIGHT OF THE JOURNAL IN WHICH THEY WERE PUBLISHED. AS SUCH, THE VARIOUS PUBLISHING COMPANIES RETAIN ALL RIGHTS TO REPRODUCE AND DISTRIBUTE THESE ARTICLES – INCLUDING REPRINTS, TRANSLATIONS, PHOTOGRAPHIC REPRODUCTIONS, MICROFORM, ELECTRONIC FORM (OFFLINE, ONLINE), OR ANY OTHER REPRODUCTIONS OF SIMILAR NATURE.
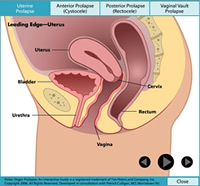
Prolapse Animation
Treatments for Prolapse
Subjective and objective outcomes 1 year after robotic-assisted laparoscopic sacrocolpopexy
Abstract: We aimed to assess the subjective and objective outcomes 1 year after robotic sacrocolpopexy using a type I polypropylene mesh. This was a case series of 64 patients who underwent a robotic-assisted laparoscopic sacrocolpopexy using a type I monofilament polypropylene mesh coated with hydrophilic porcine collagen. Objective and subjective outcomes were assessed using the pelvic organ prolapse quantification (POP-Q), the short forms of the Pelvic Floor Impact Questionnaire (PFIQ 7) and the Pelvic Floor Distress Inventory (PFDI-20). Outcome measures were collected pre-operatively and 1 year post-operatively on all but one patient, who was lost to follow-up. Paired comparisons between pre- and post-operative outcomes were performed using the Wilcoxon signed rank test. At 1 year, POP-Q stage II or greater and loss of follow-up were considered to be surgical failure. The “surgical cure” rate was 89%. We observed three distal anterior failures, two distal posterior failures and one apical failure, and one patient was lost to follow-up. We found significant differences between pre- and post-operative POP-Q measurements (p < 0.001) and PFDI-20/PFIQ-7 total scores (p < 0.001). Robotic sacrocolpopexy using this polypropylene mesh resulted in significant improvements in subjective and objective outcome measures at 1 year.
Sexual function before and 1 year after laparoscopic sacrocolpopexy
Abstract: This study aimed to compare sexual function before and 1 year after laparoscopic sacrocolpopexy using a porcine dermis or a polypropylene mesh material. This was a secondary analysis of sexual function measured before and after laparoscopic sacrocolpopexy in a group of 81 sexually active women participating in a randomized controlled trial comparing porcine dermis and polypropylene mesh. Sexual function was assessed using the short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Responses to individual questions from the physical domain of the PISQ-12 were also analyzed. Additional information included the type of mesh material used and whether a concomitant suburethral sling or perineorrhaphy was performed. There was a significant postoperative improvement in total PISQ-12 scores for the entire cohort. Similarly, PISQ-12 scores were significantly improved in both groups at 1 year. There were no differences between the 2 graft material groups. Preoperatively, 63.0% (48/76) of women reported avoiding sexual intercourse because of bulging in vagina (PISQ-12 question #8), at 1 year postoperatively only 4% (3/76) had a positive response. We observed a significant decrease in the number of women who reported pain during intercourse at 12 months as evidenced by the responses to PISQ-12 question #5, 47.4% (36/76) versus 26.3% (20/76). The addition of a suburethral sling or a perineorrhaphy did not negatively impact sexua function at 1 year. In conclusion, we found that laparoscopic sacrocolpopexy had a positive impact on sexual function at 1 year regardless of whether a porcine dermis or a polypropylene mesh material was used.
Prospective cohort study of bowel function after robotic sacrocolpopexy
Abstract: To determine bowel function changes after robotic sacrocolpopexy. Prospective data were collected preoperatively, 6 months and 12 months postoperatively. Primary outcome measures were Colorectal-anal Distress Inventory, Short Form 8 (CRADI-8) and Colorectal-anal Impact Questionnaire, Short Form 7 (CRAIQ-7) total scores. Patient reported “splinting to defecate” was followed independently. Postoperatively, we categorized patients as ‘improved’, ‘unchanged’, or ‘worsened’ using the minimum clinically important difference (MCID) of CRADI-8 scores. Of 423 consecutive patients who underwent robotic-sacrocolpopexy at our institution between 2007 and 2011, 393 (93%) completed 12 month follow up. Mean CRADI-8 scores at baseline, 6 months and 12 months were 21.1±20, 8.3±12, and 7.3±11 respectfully (p<0.0001). Mean CRAIQ-7 scores at baseline, 6 months and 12 months were 11.1±20, 3.7±13, and 2.4±9 respectfully (p<0.0001). Preoperatively, 152 patients reported a need to splint the vagina or perineum to complete a bowel movement. At 12 months, 70% of these “splinters” reported resolution of that problem. Twenty-two patients reported de-novo splinting at 12 months. Nevertheless, these de-novo splinters reported low degree of bother (CRADI-8 score 13.2±9). Using MCID of 10 points, bowel function improved for 45% of patients, was unchanged for 51% and worsened for just 4%. Those classified as improved had the worst preoperative CRADI-8 scores (mean 36.5±18) while those classified unchanged or worsened reported little bother to begin with (CRADI-8 mean scores 8±10 and 10±15 respectfully). Robotic sacrocolpopexy was associated with significant improvements in all aspects of bowel function measured by CRADI-8 and CRAIQ-7.
Cost effective analysis comparing robotic sacrocolpopexy to a vaginal mesh hysteropexy
Abstract: To compare costs and QoL associated with 2 minimally invasive operations to treat uterovaginal prolapse. A decision analytic cost-effectiveness model comparing vaginal mesh hysteropexy to robotic-assisted sacrocolpopexy. Costs were derived from a hospital perspective. QoL estimates focused on: recurrent prolapse; erosion; infection; transfusion; cystotomy; chronic pain; lower urinary tract symptoms; and mortality. Actual procedural costs at our institution were calculated. Costs and quality adjusted life years were examined over 1 year. The costs ($21,853) and QALYs (0.9645) for robotic sacrocolpopexy produced a CE Ratio of $22,657 per QALY. The costs ($14,890) and QALYs (0.9309) for vaginal mesh produced a CE Ratio of $15,995 per QALY. The incremental cost per QALYs for robotic surgery was $207,232. Sensitivity analysis on all utilities, cost estimates, and complication estimates didn’t cross any thresholds. Vaginal mesh was more cost-effective than robotic sacrocolpopexy even when the cost of the robot was not factored in.
Subjective and objective results 1 year after robotic sacrocolpopexy using a lightweight Y-mesh
Abstract:To assess outcomes following robotic sacrocolpopexy using an ultra-lightweight polypropylene Y-mesh. During our study period, all patients who underwent robotic sacrocolpopexy were enrolled in this single-arm prospective trial. Endpoints included POP-Q values; Pelvic Floor Distress Inventory, Short Form 20 (PFDI-20); Pelvic Floor Impact Questionnaire, Short Form 7 (PFIQ-7); Surgical Satisfaction scores; and the Sandvik Incontinence Severity Index. All surgeries were performed with a pre-configured monofilament type-1 polypropylene Y-mesh (Alyteã CR Bard, Covington, GA). Cure rates at 12 months were calculated using two separate definitions: 1) “clinical cure”: no POP-Q points > 0; Point C £ -5; no prolapse symptoms on the PFDI-20; and no re-operations for prolapse. 2) “objective anatomic cure”: POP-Q stage 0 or 1; Point C of £ -5; and no re-operations for prolapse. 150 patients underwent robotic sacrocolpopexy and 143 (95%) were available for 12-month follow-up. Mean age was 58.6 ± 9.8 and mean BMI was 26.3 ± 4.5. Mean operative time and blood loss were 148 ± 27.6 minutes (range 75-250 minutes) and 51.2 ± 32 respectively. There were no mesh erosions or exposures, and mesh edges were not palpable in any patient.
Prospective study of an ultra-lightweight polypropylene Y-mesh
The purpose of our study was to prospectively evaluate the use of a particular polypropylene Y mesh for robotic sacrocolpopexy. This was a prospective study of 120 patients who underwent robotic sacrocolpopexy. We compared preoperative and 12 month postoperative objective and subjective assessments via the Pelvic Organ Proplase Quantification (POP-Q), the Pelvic Floor Distress Inventory, Short Form 20 (PFDI-20); the Pelvic Floor Impact Questionnaire, Short form 7 (PFIQ-7); and the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire 12 (PISQ-12). Objective “anatomical success” was defined as POP-Q stage 0 or 1 at all postoperative intervals. We further defined “clinical cure” by simultaneously considering POP-Q points and subjective measures. To be considered a “clinical cure”, a given patient had to have all POP-Q points ≤0, apical POP-Q point C ≤5, no reported pelvic organ prolapse symptoms on the PFDI-20, and no reoperation for prolapse at all postoperative intervals. Of the 120 patients, 118 patients completed the 1 year follow up. The objective “anatomical success” rate was 89% and the “clinical cure” rate was 94%. The PFDI-20 mean score improved from 100.4 at baseline to 21.0 at 12 months; PFIQ-7 scores improved from 61.6 to 8.0; and PISQ-12 scores improved from 35.7 to 38.6. No mesh erosions or mesh-related complications occurred. The use of this ultra-lightweight Y mesh for sacrocolpopexy, eliminated the mesh-related complications in the first postoperative year, and provided significant improvement in subjective and objective outcomes.
Porcine dermis compared with polypropylene mesh for laparoscopic sacrocolpopexy
Abstract: Our objective was to compare the surgical outcomes 12 months after laparoscopic sacrocolpopexy performed with porcine dermis and the current gold standard of polypropylene mesh. Patients scheduled for laparoscopic sacrocolpopexy were eligible for this randomized controlled trial. Both our clinical research nurse and the patients were blinded as to which material was used. Our primary endpoint was objective anatomic cure defined as no pelvic organ prolapse quantification (POP-Q) points stage 2 or greater at any postoperative interval. Our sample size calculation called for 57 patients in each group to achieve 90% power to detect a 23% difference in anatomic cure at 12 months. Our secondary endpoint was clinical cure. Any patient with POP-Q point greater than zero, or point C less than or equal to -5, or any complaints of prolapse symptoms whatsoever on Pelvic Floor Distress Inventory-20 or Pelvic Floor Impact Questionnaire, Short Form 7, or reoperation for prolapse were considered “clinical failures”; the rest “clinical cures”. Statistical comparisons were performed using the x2 or independent samples t test as appropriate. As expected, there were no preoperative differences between the porcine (n=57) and mesh (n=58) groups. The 12-month objective anatomic cure rates for the porcine and mesh groups were 80.7% and 86.2%, respectively, and the “clinical cure rates” for the porcine and mesh groups were 84.2% and 89.7%, respectively. Pelvic Floor Distress Inventory-20 and Pelvic Floor Impact Questionnaire, Short Form 7 score improvements were significant for both groups with no major differences found between groups. In conclusion, we found similar outcomes in subjective or objective results 12 months after laparoscopic sacrocolpopexy performed with either porcine dermis or polypropylene mesh.
Nonsurgical Management of Pelvic Organ Prolapse
Abstract: Although surgical management of symptomatic pelvic organ prolapse (POP) is common and often necessary, conservative treatments such as pessaries, pelvic floor muscle training, or both can usually result in symptomatic improvement. When treating patients with POP, health care practitioners should focus primarily on identification and alleviation of POP-related symptoms. It is appropriate to offer nonsurgical management to most people with POP. This article reviews the objective and subjective evaluation and nonsurgical management of POP, emphasizing a simple, practical approach to pessary fitting and management.
Evaluation of The Avaulta trans-vaginal mesh for correction of pelvic organ prolapse
Abstract: OBJECTIVE: We sought to track objective and subjective outcomes >1 year after transvaginal mesh system to correct prolapse. STUDY DESIGN: This was a retrospective cohort study of 120 women who received a transvaginal mesh procedure (Avaulta Solo, CR Bard Inc,). Outcomes were pelvic organ prolapse quantification values; Pelvic Floor Distress Inventory, Short Form 20/Pelvic Floor Impact Questionnaire, Short Form 7 scores; and a surgical satisfaction survey. “Surgical failure” was defined as pelvic organ prolapse quantification point >0, and/or any reports of vaginal bulge. RESULTS: Of 120 patients, were followed up for a mean of 14.4 months. In all, 74 patients had only anterior mesh, 21 only posterior mesh, and 21 both meshes. Surgical cure rate was 81%. Surgical failure was more common if preoperative point C >+2 (35% vs 16%; P _ .04). Mesh erosion and de novo pain occurred in 11.7% and 3.3%, respectively. Pelvic Floor Distress Inventory, Short Form 20/Pelvic Floor Impact Questionnaire, Short Form 7 scores improved. CONCLUSION: Objective and subjective improvements occurred at >1 year, yet failure rates were unacceptably high for women with the most severe cases of prolapse.
Robotic Sacrocolpopexy – Optimizing Efficiency
Abstract: Since it was first described by Lane nearly 50 years ago, the sacrocolpopexy procedure has evolved tremendously. Once a relatively morbid open abdominal procedure, this operation is now routinely performed laparoscopically, either with or without robotic assistance. Two recent studies support the use of robotic assistance for sacrocolpopexy. In 2005 our team began a transition away from traditional laparoscopic techniques toward the use of robotic assistance for these cases. Having now performed more than 300 robot-assisted laparoscopic sacrocolpopexies, we have adopted some new time-saving techniques that do not involve shortcuts that may change the nature of the procedure (such as the use of staples). In 2008, we published a detailed description of our robotic techniques in this journal. The purpose of this month’s article is to provide an update that includes our newest surgical improvements. Video of the procedure is available on YouTube at www.youtube.com/watch?v=ScVlmysgsC4 to further illustrate our descriptions.
5 year results of a randomized trial comparing fascia lata and synthetic mesh for sacrocolpopexy
Abstract: Introduction and hypothesis: The purpose of this study is to evaluate the 5-year surgical outcomes of abdominal sacrocolpopexy among subjects randomized to receive polypropylene mesh or cadaveric fascia lata. Methods: All 100 subjects from the original randomized clinical trial were eligible. Primary outcome was objective anatomic failure: any pelvic organ prolapse quantification (POP-Q) point >=-1. Secondary outcome was clinical failure—presence of bulge or prolapse symptoms and either a POP-Q point C>=½ TVL or any POP-Q point >0—and interim surgical re-treatment. Wilcoxon tests and Fisher’s exact test were performed. Results: Fifty-eight subjects returned for 5-year follow-up— 29 mesh and 29 fascia. Objective anatomic success rates were: mesh, 93% and fascia, 62%. Clinical success rates were: mesh, 97% and fascia, 90%. Conclusions: Polypropylene mesh was superior to cadaveric fascia lata using objective anatomic outcomes. Success rates of mesh and fascia were comparable using a clinical definition that combined symptoms with anatomic measures.
Options and Techniques for Prolapse repair
Abstract: Options for treatment of pelvic floor prolapsed continue to evolve; however, questions regarding the etiology of prolapse remain unanswered. Clearly related to such factors as childbirth and the aging process. Prolapse is likely to become of greater concern to clinicians as the population of women aged 60 years and older increases. Its incidence is expected to reach or exceed 30% in this age-group. The demand for gynecologic services likely will increase by more than 45% in the next 10 years. Prolapse is also associated with defects in collagen and smooth-muscle structure and strength. Tissue may weaken in response to physical activity or increased intra-abdominal pressure from chronic constipation, chronic cough, chronic obstructive pulmonary disease, or obesity. This roundtable discussion among experts examines the medical evidence regarding the etiology and management of prolapse, evaluates currently available treatments, and describes emerging trends.
The choice of prolapse treatments
Abstract: OBJECTIVE: To evaluate which clinical factors were predictive of treatment choice for patients with pelvic organ prolapse. METHODS: One hundred fifty-two patients were enrolled in this cross-sectional study to collect clinical data on potential predictors of treatment choice. Continuous parametric, continuous nonparametric (ordinal), and categoric data were compared with chosen management plan (expectant, pessary, surgery) using analysis of variance, the Kruskal– Wallis test, and the _2 test for association, respectively. All significant predictors of treatment choice for pelvic organ prolapse identified during univariate analysis were entered into a backward elimination polytomous logistic regression analysis for predicting surgery versus pessary versus expectant management, with surgery as the reference group. RESULTS: The probability of choosing expectant management rather than surgery 1) increases as the preoperative pelvic pain score increases and 2) decreases as the prolapse severity increases. The probability of choosing pessary rather than surgery 1) increases as age increases and 2) decreases as the prolapse severity increases and 3) is less if the participant had prior prolapse surgery. CONCLUSION: Age, prior prolapse surgery, preoperative pelvic pain scores, and pelvic organ prolapse severity were independently associated with treatment choices in a predictable way and provide physicians with medical evidence necessary to support a patient’s decision.
The anterior approach to sacrospinous ligament suspension
Abstract: OBJECTIVE: To compare vaginal anatomy and sexual function after the conventional posterior and anterior sacrospinous vault suspension. METHODS: A retrospective repeated measures cohort study included all 168 consecutive sacrospinous vault suspension procedures between July 1990 and February 1997. The posterior suspension used a posterior vaginal incision and pararectal dissection. Anterior suspension involved an anterior rather than posterior vaginal incision, retropubic perforation, and dissection of a paravaginal-paravesical rather than pararectal space to accommodate the vaginal vault. Two polytetrafluoroethylene sutures anchored the anterior vaginal cuff (for the anterior sacrospinous suspension) or the posterior vaginal cuff (for the posterior sacrospinous suspension) to the ligament. Postoperative evaluation included an examination using the pelvic organ prolapse quantitative system, assessment of vaginal width and axis, and symptom questionnaire. RESULTS: Total vaginal length and apical suspension were slightly greater after the anterior suspension, and recurrent anterior vaginal relaxation was less likely. No differences were found in maximal dilator size or apical narrowing between the two groups. New onset dyspareunia was reported by two subjects in the anterior vault suspension group, and two in the posterior vault suspension group. Three of these four cases of de novo dyspareunia were attributable to either severe atrophy or recurrent prolapse, and none to vaginal narrowing or shortening. CONCLUSION: After anterior sacrospinous vault suspension, vaginal length and apical suspension were slightly increased, and recurrent anterior vaginal prolapse decreased compared with the posterior sacrospinous suspension technique. Upper vaginal caliber and sexual function appear well preserved using either technique.
Surgical repair of the posterior compartment
Abstract: The support anatomy of the posterior vaginal wall is a byproduct of complex interactions among the pelvic floor muscles, nerves, and connective tissue. Before a surgeon can successfully plan and perform an operation to correct a posterior compartment defect, he or she must understand not only the anatomic principles outlined in chapter 1 of this text, but the methods for assessing prolapse symptoms outlined in chapter 4 as well. Generally, surgical intervention is only considered when 1) a posterior compartment defect produces symptoms (such as pressure, heaviness, pain, incomplete rectal emptying, and so on) or 2) when other significant prolapse is present. The connective tissue layer of the posterior vaginal wall, commonly referred to as the rectovaginal septum, runs laterally to the pelvic sidewall and fuses distally to the perineal body. A full description of the posterior wall anatomy is covered in chapter 1 of this text. For the purposes of this chapter, the term vaginal muscularis is used to refer to the ”fascial” tissue that attaches to the pelvic sidewall. Stretching and/or tearing of this layer are generally considered the fundamental occurrence that results in posterior wall support defects. Although this chapter focuses on posterior wall surgery, it is important for the pelvic surgeon to recognize and address any other defects (especially apical descent) when planning surgery for a particular patient. In fact, some operations primarily aimed to correct apical prolapse—such as the sacral colpopexy (discussed in chapter 8)— can actually correct posterior wall prolapsed at the same time. Nonetheless, this chapter strictly focuses on the various methods for surgically addressing the posterior compartment— focusing on the medical evidence supporting each operation.
Long-term results of sacral colpopexy
Abstract: OBJECTIVE: The aim was to determine the minimum meaningful study period required for prospective trials involving sacral colpopexy. STUDY DESIGN: This is a retrospective analysis of 245 patients who underwent sacral colpopexy. Postoperative pelvic organ prolapse quantitation was our objective end point. In an effort to control for selection bias, patients who returned for postoperative examinations were compared with those who did not for clinical and demographic information. A validated prolapse-specific quality of life instrument was used to determine the subjective end points. RESULTS: Objective failure (any postoperative POP-Q point >= stage II) was found in 37 (15.1%) patients. Of these, 26 (70.3%) occurred within 6 months, and 30 (81.1%) occurred within 1 year. Another 5 objective failures were discovered between 1 and 2 years after surgery for a total of 94.6% of failures occurring within 2 years. There were no clinically significant differences between the groups of women with and without objective postoperative follow-up, indicating minimal selection bias. CONCLUSION: It is reasonable to construct randomized controlled trials involving sacral colpopexy that only include 1- or 2-year follow-up, because almost all “failures” happen within that time frame.
A randomized controlled trial of Vicryl mesh to prevent prolapse
Abstract: OBJECTIVE: Our aim was to evaluate the efficacy of polyglactin 910 mesh in preventing recurrent cystoceles and rectoceles. STUDY DESIGN: In a prospective, randomized, controlled trial, patients undergoing vaginal reconstructive surgery with cystoceles to the hymenal ring and beyond were randomly selected to undergo anterior and posterior colporrhaphy with or without polyglactin 910 mesh reinforcement. Results were evaluated preoperatively and at 2, 6, 12, and 52 weeks postoperatively. RESULTS: A total of 161 women were randomly selected for this study. One woman was excluded at the time of surgery, and 17 women were lost to follow-up. Eighty women received mesh, and 80 did not. Both groups were found to be equivalent with respect to age, parity, concomitant surgery, and menopausal and hormone replacement status. Preoperatively 49 women had a central cystocele to the hymenal ring and 111 women had cystoceles beyond the introitus; 91 women had a rectocele to the mid-vaginal plane, 31 to the hymenal ring, and 22 beyond the introitus. After 1 year, 30 of 70 subjects without mesh and 18 of 73 subjects with mesh had recurrent cystoceles beyond the mid-vaginal plane. Eight women without mesh and 2 women with mesh had recurrent cystoceles to the hymenal. No recurrent cystoceles beyond the hymenal ring occurred in either group. Multivariate logistic regression analysis showed concurrent slings to be associated with significantly fewer recurrent cystoceles whereas the presence of mesh remained significantly predictive of fewer cystocele recurrences in this analysis. Thirteen recurrent rectoceles were noted 1 year postoperatively, with no differences between groups. CONCLUSION: Polyglactin 910 mesh was found to be useful in the prevention of recurrent cystoceles.
A randomized blinded trial comparing mesh and fascia lata for sacral colpopexy
Abstract: Objective: To compare the objective anatomic outcomes after sacral colpopexy performed with cadaveric fascia lata and polypropylene mesh. Methods: Patients undergoing a sacral colpopexy were randomized to receive either fascia lata or polypropylene mesh in a double-blinded fashion. Data were collected at 6 weeks, 3 months, 6 months, and 1 year postoperatively. The main outcome measures were pelvic organ prolapsed quantification (POP-Q) system stage and individual POP-Q points over time. Objective anatomic failure was defined as POP-Q stage 2 or more at any point during the follow-up period. Proportions of patients with objective anatomic failure at 1 year in each group were compared using the X2 test. Mean POP-Q points and stage at 1 year were compared by using the independent samples t test. Results: One hundred patients were randomized to receive either fascia or mesh. Of the 89 patients returning for 1-year follow-up, 91% of the mesh group and 68% of the fascia group were classified as objectively cured. We found significant differences between the mesh and fascia groups with respect to the 1-year postoperative comparisons of points Aa, C, and POP-Q stage. There were no differences between the 2 groups with respect to points TVL (total vaginal length), GH (genital hiatus), PB (perineal body), Ap or Bp (2 points along the posterior vaginal wall). Conclusions: Polypropylene mesh was superior to fascia lata in terms of POP-Q points, POP-Q stage, and objective anatomic failure rates. Cadaveric fascia lata is not a good choice for this operation.
Abstract: Last fall, during a meeting of the ACOG Gynecologic Practice Committee, an FDA official was made aware of the current controversy surrounding vaginal mesh placement to correct pelvic organ prolapse. Three weeks later, on October 20th, the FDA issued a public health notification entitled “Serious Complications Associated with Transvaginal Placement of Surgical Mesh in Repair of Pelvic Organ Prolapse and Stress Urinary Incontinence.” This document made reference to “over 1,000 reports from nine surgical mesh manufacturers of complications associated with [vaginal] surgical mesh” and went on to list specific complications, such as mesh erosion through the vaginal epithelium, infection, pain, urinary problems, and prolapse recurrence.
Abstract: Note: This article is a continuation from the April issue in which 7 vaginal mesh systems were described. Mesh systems were developed to create effective and highly reproducible vaginal prolapse procedures. However, the paucity of long-term clinical data regarding these systems places the burden of choosing whether to use them squarely on the “surgeon-gatekeeper.”
Abstract: Robotic surgery represents the latest development in gynecologic laparoscopy, enabling surgeons to use a minimally invasive approach for more complex procedures.
Relationship between prolapse and back pain
Abstract: OBJECTIVE: To test the null hypothesis that there is no association between pelvic organ prolapse and pelvic or low back pain. METHODS: A total of 152 consecutive patients with pelvic organ prolapse completed a visual faces scale to quantify the amount of pelvic or low back pain present. Pelvic organ prolapse severity was graded by three techniques: 1) pelvic organ prolapse quantification staging; 2) descent of the leading edge of prolapse; and 3) dynamic cystoproctography. Linear and nonlinear associations of pelvic organ prolapse quantification staging, descent of the leading edge of prolapse, and dynamic cystoproctography findings with pelvic or low back pain were assessed. We also characterized the nature of any significant nonlinear associations. RESULTS: Descent of the leading edge of prolapse was linearly associated with low back pain. Patients with greater descent of the leading edge of their prolapse reported less low back pain. Bladder descent during dynamic cystoproctography was nonlinearly associated with low back pain. Neither of these associations was statistically significant after controlling for patient age and prior prolapse surgery. There were no linear or nonlinear associations between pelvic organ prolapse and pelvic pain. CONCLUSION: Based on the data, pelvic organ prolapse is not a cause of pelvic or low back pain.
Treatments for Incontinence
A prospective study of a single incision sling at the time of robotic sacrocopoplexy
Abstract: The objective of this study was to evaluate the efficacy and safety of the Miniarc Precise® single incision sling (American Medical Systems, Minnetonka, MN) placement at the time of a robotic sacrocolpopexy. This was a prospective study of a single incision suburethral sling placed at the time of robotic Sacrocolpopexy in women with stress urinary incontinence (SUI) and pelvic organ prolapse. Primary outcome measure was cure at one year, defined objectively by a negative cough stress test (CST) and subjectively by a score of ‘0 or 1’ on question 17 of the Pelvic Floor Distress Inventory (PFDI-20) “Do you experience urine leakage related to coughing/sneezing/laughing”. Secondary outcome measures included the change in Urinary Distress Inventory (UDI-6) and Urinary Impact Questionnaire (UIQ-7) scores at 1 year. All sling-related complications were reported. Paired Student’s t test was used for statistical analysis. 101 patients were included between August 2010 and July 2012. One year follow-up was available for 97/101 patients (96%). Objective cure was 90% and subjective cure was 87%. Baseline UDI-6 scores improved from 32.5±23 to 5.4±10 at 1 year (p<0.001). Similarly, baseline UIQ-7 scores improved from 21.2±23.9 to 2.3±6.9 at 1 year (p<0.001). There were no intraoperative cystotomies, no mesh erosions, no sling revisions and no cases of urinary retention. The addition of a single incision suburethral sling at the time of robotic sacrocolpopexy in women with SUI resulted in an 87% cure rate at 1 year.
Validity of Incontinence Severity Index
Abstract: Aims: To assess the construct validity of the incontinence severity index (ISI) by testing its correlation with two health-related quality of life measures, the short forms of the Urogenital Distress Inventory (UDI-6) and the Incontinence Impact Questionnaire (IIQ-7), in women with urodynamic stress incontinence. Materials and Methods: A cohort of 170 women with the urodynamic stress incontinence who underwent corrective surgery completed the ISI, IIQ-7, and the UDI-6 both pre and post-treatment. We correlated the pre- and post-treatment responses between the ISI, the IIQ-7, the UDI-6 and their subscales. We also assessed the sensitivity of the ISI to change by correlating the percent change in score between the three instruments. The results were analyzed using a non-parametric test of correlation, the Spearman’s rho. Results: The ISI scores were generally not well correlated with the pre-treatment IIQ-7 and UDI-6 scores. The post-treatment scores and percent change from pre- to post-treatment of the ISI, however, were highly correlated with that of the IIQ-7 and UDI-6. The ISI was most highly correlated with the UDI-6 stress symptoms subscale and most poorly correlated with the UDI-6 obstructive/discomfort subscale. Conclusions: This study provides valuable insight into the construct validity of the ISI. Evidence of its convergent validity is found in the high correlation with the stress symptoms subscales of the UDI-6, while the poorer correlation with the obstructive subscale provides evidence of its divergent validity. These data also suggest that the ISI is highly sensitive to change seen with treatment.
Case Report regarding obturator and retropubic slings
Abstract: The transobturator sling procedure is a relatively new technique as compared to the retropubic version. The functional differences between these two procedures are largely unknown. Two cases of failed transobturator slings are reported. In both cases, the procedure was done under local anesthesia and a cough stress test was performed to adjust the tape. The transobturator slings were unable to stop the leakage and we replaced them with the retropubic versions, which were successful. Even when pulled very tightly, some transobturator slings will fail to stop stress incontinence that is amenable to cure from a typically placed “tension-free” retropubic sling. The cough stress test can identify such cases.
Pelvic organ prolapse following a Burch procedure
Abstract: The purpose of our study was to examine the incidence of prolapse in a group of women who had had an isolated Tanagho modification of the Burch colposuspension performed without significant pelvic organ prolapse preoperatively. Sixty women were identified who underwent an isolated Burch procedure for genuine stress incontinence between 1991 and 1999. Thirty-four women returned for postoperative Pelvic Organ Prolapse Quantification (POP-Q) staging evaluation. Overall, 6 had stage II anterior prolapse. Eleven had stage II posterior prolapse. Three had stage II uterine prolapse. None of these patients with identified support defects was symptomatic. Two patients had subsequently undergone vaginal hysterectomy. One had this performed for dysfunctional uterine bleeding 3 years after her Burch procedure. One patient developed symptomatic uterine prolapse and underwent a vaginal hysterectomy 5 months after her Burch procedure. The majority of patients undergoing an isolated Tanagho modification Burch procedure without preoperative prolapse do not appear to be placed at increased risk for subsequent operative intervention.
Evaluation and treatment of female urinary incontinence
Abstract: Urinary incontinence in women is a common problem and one that will increase in prevalence as the population ages. This condition can be categorized into three basic types: stress, urge, and mixed incontinence. Careful history taking and a comprehensive physical exam will provide the diagnosis in many cases. With the proper knowledge base, physicians can counsel their patients on the various forms of treatment for incontinence, which range from completely noninvasive behavioral therapies to surgical management. This article offers a basic guideline for the evaluation and treatment of female urinary incontinence.
case reports – osteomyelitis following bone anchor placement
Abstract: We report on four patients who had a retropubic abscess (three with osteomyelitis) with involvement of the adjacent soft tissues following a procedure to correct stress urinary incontinence with use of pelvic bone screws to serve as anchors for sutures that were placed to support the bladder neck. The ages of the patients ranged from seventy-one to eighty years old. None of the patients had a known previous urinary tract infection. Two of the procedures were performed at our institution, and two were performed at different outside institutions. The patients were seen because of suprapubic pain, swelling, and erythema between four and twenty-four weeks after the procedure. Two had received courses of orally administered antibiotics because of wound drainage within a week to ten days after the original procedure. Computerized tomography scans of the pelvis showed soft-tissue swelling behind the symphysis pubis and erosion of the adjacent bone. The abscess was drained in all patients, and infected bone was excised, with removal of a total of two to three centimeters of bone, in three patients. In all patients, the sinus tract was excised, extensive soft-tissue debridement was performed, and the suspension sutures and bone anchors were removed. In one patient, debridement was necessary on two occasions. Cultures were positive for Pseudomonas aeruginosa and Staphylococcus aureus in one patient, Pseudomonas aeruginosa and coagulase-negative Staphylococcus in one patient, Staphylococcus aureus in one patient, and Citrobacter species and a gram-positive coccus in one patient. Each of the four patients was managed intravenously with antibiotics, with the dosage determined according to her age and renal function, for six weeks. Suspension of the bladder with use of pelvic screws as suture anchors may increase the risk of osteomyelitis because the screwsuture combination passes through the vaginal lumen before it is anchored into bone.
Incidence of pubic osteomyelitis following bone anchor placement
Abstract: Objectives. To determine the incidence of pubic osteomyelitis after bladder neck suspension using suprapubic bone anchors. Methods. The target population consisted of 290 consecutive women who underwent bladder neck suspension using suprapubic bone anchors between June 1994 and November 1999 at two referral centers. A structured telephone questionnaire was designed to elicit any history of clinical symptoms suspicious for pubic osteomyelitis. Positive responses were followed up by a detailed review of the medical records. Nonresponders were evaluated by chart review, with negative cases included only if the documented follow-up reached 1 year. Results. The sample consisted of 225 women, representing 77.6% of the study population, with a mean age of 69.7 years and a mean follow-up of 31.8 months. Of the 225 women, 179 completed the telephone survey; 46 patients were evaluated by long-term chart review. Three patients reported positive responses to the screening questionnaire and were confirmed to have developed pubic osteomyelitis. Each had undergone exploratory laparotomy, anchor removal, bony debridement, and prolonged parenteral antibiosis. The most common noninfectious complaints were irritative voiding symptoms and pubic or groin pain responding to “conservative” therapy (3.5%), including 1 case of osteitis pubis. One subject underwent repeated operation because of erosion of the sling sutures into the bladder. Conclusions. The estimated incidence of osteomyelitis after bone-anchored bladder neck suspension was 1.3%. Although postoperative osteomyelitis is rare, each case incurs substantial morbidity and a complicated postoperative course.
The protective effect of slings against anterior vaginal wall prolapse
Abstract: OBJECTIVE: The purpose of this study was to evaluate the independent effect of suburethral sling placement on the risk of cystocele recurrence after pelvic reconstructive operation. STUDY DESIGN: One hundred forty-eight women with cystoceles to or beyond the hymenal ring underwent pelvic reconstructive operation, with or without incontinence procedures, and were evaluated at 12 and 52 weeks after operation with a standardized pelvic examination. Rates of recurrent prolapse, at all sites, were statistically compared between subjects with and without suburethral slings. A multiple regression analysis was used to determine the independent effect of sling placement on the risk of recurrent cystoceles. RESULTS: Suburethral sling placement was associated with a 54.8% reduction in the mean rate of postoperative cystocele recurrence. This protective effect was observed as early as 12 weeks and remained significant at 1-year follow up. A markedly reduced risk of cystocele recurrence was observed when women with sling procedures were compared with all other women, with those women who underwent other incontinence operations, and even with those women who had undergone prolapse repair with no incontinence procedure. The protective effect of the sling procedure remained highly significant, even after controlling for potentially confounding variables in a multiple logistic regression model. CONCLUSION: Suburethral sling procedures appear to significantly reduce the risk of cystocele recurrence after pelvic reconstructive operation, in contrast with the effect of retropubic urethropexy and needle suspensions. These findings should be considered when the surgical treatment of stress incontinence that accompanies pelvic organ prolapse is being planned.
The effects of Anesthesia on voiding function after a TVT procedure
Abstract: OBJECTIVE: To determine whether the mode of anesthesia used during the tension-free vaginal tape procedure affects postoperative voiding function. METHODS: A retrospective cohort study was performed using cases in which tension-free vaginal tape placement was the sole procedure performed. Of the 173 cases reviewed, we were able to use the data from 163. Hierarchal linear regression was used to identify independent predictors of our dependent variable: days to complete voiding. In the first block, established predictors of postoperative voiding dysfunction were entered into the model. In the second block, potential confounders of the relationship between anesthesia type and days to complete voiding identified during univariate analysis were entered into the model. In the third block, anesthesia type was entered into the model to determine whether it added any unique variance after controlling for previously established predictors of postoperative voiding dysfunction. RESULTS: The mean days to complete voiding was similar in our local or regional anesthesia and general anesthesia groups. Our final regression model included age, prior pelvic organ prolapse surgery, and preoperative urge symptoms and explained 22.2% of the variance in days to complete voiding. Anesthesia type did not add any predictive improvement after controlling for these variables. CONCLUSION: General anesthesia, and therefore lack of a cough-stress test, does not increase the chance of postoperative voiding dysfunction associated with tension-free vaginal tape.
Randomized controlled trial of Burch versus sling
Abstract: The aim of this study was to compare the long term results of a modified Burch procedure with a sling procedure for the treatment of stress incontinence with a low-pressure urethra. Thirty-six women with urodynamic stress incontinence, low-pressure urethra, urethral hypermobility and no significant pelvic organ prolapsed were randomly assigned to undergo either a modified Burch procedure or a sling placement . Cure of the stress incontinence (defined as a negative stress test and negative pad-weight test) was the primary long-term endpoint. Secondary endpoints included subjective cure of stress incontinence (defined as no incontinence episodes on a 1-week voiding diary) and voiding function studies. Comparisons of group means were performed with the Mann–Whitney U-test, pooled variance t-tests and separate variance t-tests. Proportions were compared with Fisher’s exact test. A logistic regression analysis was performed to control for covariates that differed in our two groups despite randomization. Long-term follow-up (mean=72.6 months) was available for 82% of the original study group. The objective cure rates for the Burch and sling groups were 84.6% and 100%, respectively. Mean uroflowmetry rates for the Burch and sling groups were 7.38 and 6.8 ml/s, respectively. Mean postvoid residual volumes for both groups were 35 ml. Two sling patients (12%) required partial resection of their slings because of erosion. Both patients remained continent. In terms of voiding function and stress incontinence cure, there were no differences between groups undergoing modified Burch or sling procedures for treatment of urodynamic stress incontinence with low-pressure urethra.
Randomized controlled trial of Burch versus sling – LONG TERM RESULTS
Abstract: OBJECTIVE: The aim of this study was to compare a modified Burch procedure with a suburethral sling for the treatment of stress incontinence complicated by a low-pressure urethra. STUDY DESIGN: Thirty-six women with stress incontinence, low-pressure urethra, and urethral hypermobility (straining cotton swab angle >=30°) were randomly assigned to undergo either a modified Burch procedure (n = 19) or a suburethral sling (n = 17). Objective and subjective cure rates at 3 months after the operation were the primary outcome measures. Comparisons of group means were performed with the Student t test for independent groups, and proportions were compared with the Fisher exact test. RESULTS: After the operation the 2 groups had statistically similar cure rates and voiding function. Urethral closure pressure, pressure transmission ratios, and maximum detrusor pressure during voiding were significantly higher in the sling group. CONCLUSION: At 3 months there were no clinically significant differences between the groups treated with suburethral sling and modified Burch procedures.
Urethral retro-resistance…a new urodynamic measurement
Abstract: Aims: The urethral retro-resistance pressure (URP) is a retrograde urethral pressure profile measured by a new urodynamic measurement system. URP is the pressure required to achieve and maintain an open sphincter. This clinical investigation focused on a comparison of URP to standard urodynamic measurements and an examination of their relationship to incontinence severity. Methods: Twenty-two centers enrolled 258 stress incontinent women in a randomized, crossover study of two groups: (1) test procedure followed by multichannel urodynamics, (2) multichannel urodynamics followed by test procedure. We defined incontinence severity categories using 24 hr urine loss and assessed these categories using incontinence quality of life (I-QOL), urinary incontinence severity score (UISS), incontinence visual analogue score (VAS), URP, maximum urethral closure pressure (MUCP), and leak point pressure (LPP). Results: The mean age was 56.2 years. No order effect was present. The correlation coefficient between URP and MUCP was 0.31; between URP and LPP was 0.28; and between MUCP and LPP was 0.14. The mean values for URP across symptom severity categories were significantly different and decreased with increasing severity. The mean values for MUCP and LPP did not decrease with increasing severity. Conclusions: The study demonstrated that URP had a consistent relationship with incontinence severity. The data suggested that URP is a physiological measure of urethral function and may have clinical utility as a diagnostic tool. Future outcomes-based research is necessary to establish the predictive value of URP, MUCP, and LPP measurements in terms of incontinence cure rates and diagnosis of sphincter dysfunction.
Safety of reusing GAX-collagen MULTICENTER STUDY
Abstract: We have previously reported pilot data regarding the safety of saving partially used syringes of a glutaraldehyde cross-linked collagen for use in subsequent treatment sessions with the same individual. That single institution study involved 56 partially used syringes cultured for aerobic bacteria. Only one weakly positive culture was detected among these 56 samples, which prompted us to carry out this expanded study involving multiple centers and different injection techniques. Samples were collected from four centers. Following periurethral injection in an office setting, 166 partially used syringes of glutaraldehyde cross-linked collagen were refrigerated for between 1 and 104 weeks (average 58). Material from all 166 syringes was then cultured qualitatively and quantitatively for both aerobic and anaerobic organisms. Collagen from one syringe grew >100 000 colonies of Escherichia coli. All other cultures were negative. In the pilot study, one culture of 56 syringes was weakly positive for coagulase-negative staphylococcus. When the results from both studies were considered together, only two of 222 partially used syringes were contaminated. The background risk of local infection associated with periurethral collagen injection is approximately 0.29%. Using the statistical equation ‘number needed to harm’, we found that a clinician would have to reuse 111 syringes at a saving of $34,965 before he or she would cause a single local injection. Therefore, we feel that it may be cost-effective and safe to reinject material from a partially used syringe of glutaraldehyde cross-linked collagen during a subsequent treatment session on an individual.
Safety of reusing GAX-collagen syringes
Abstract:We evaluated the safety of saving partially used syringes of glutaraldehyde crosslinked collagen for subsequent treatment sessions in an individual. Materials and Methods: After periurethral injection in an office setting 56 partially used syringes of glutaraldehyde cross-linked collagen were stored in a refrigerator for 1 to 61 weeks. Collagen from all 56 syringes was then cultured qualitatively using a broth medium at 35C and semiquantitatively using a chocolate agar plate at 22 to 30C for 5 days each. Results: A qualitative broth culture was positive for coagulase negative staphylococcus but the results of semiquantitative chocolate agar culture of material from the same syringe were negative. All cultures of the other 55 syringes were negative. Conclusions: The positive culture most likely resulted from contamination during periurethral injection or the culturing process. Minimal contamination from and the great potential cost savings of reusing glutaraldehyde cross-linked collagen for subsequent treatments in an individual indicate the need for an expanded study involving multiple centers.
Urinary Incontinence in Women: Evaluation and Management
Abstract: Because the prevalence of urinary incontinence increases with age, a working knowledge of the diagnosis and treatment of the various types of urinary incontinence is fundamental to the care of women. As the population of the United States ages, primary care physicians can expect to see an increasing number of patients with urinary incontinence. By obtaining a careful medical history and performing a comprehensive physical examination, the primary care physician can initiate successful treatment for the majority of patients without the need for invasive testing. This article offers a comprehensive approach to the evaluation and management of urinary incontinence in women.
TVT placed under local anesthesia gives better results
Abstract: OBJECTIVE: To estimate whether the mode of anesthesia (and the resultant ability or inability to perform the cough stress test) used during the tension-free vaginal tape (TVT) procedure affects postoperative continence. METHODS: A cohort of 170 women who underwent the TVT procedure without any other concomitant surgery completed the short form of the Urogenital Distress Inventory (UDI-6) to assess their continence status preoperatively and postoperatively. RESULTS: Both anesthesia groups showed significant improvement from their preoperative UDI-6 scores to their postoperative scores. However, when comparing the change from pre- to postoperative UDI-Stress Symptoms subscale scores between the 2 groups, we found a significant difference. Mean improvement in the local group was 58.3 compared with 41.7in the general group. CONCLUSION: Women who undergo TVT show significant improvements in incontinence severity regardless of anesthesia type. However, greater improvements in stress incontinence, as measured by the UDI-Stress Symptoms subscale, are seen when the TVT is placed while using the cough-stress test under local analgesia.
Comparison of microtransducer and fiber optic urodynamic catheters
Abstract: OBJECTIVE: To assess the validity and reproducibility of a fiberoptic transducer urodynamic catheter for urethral closure pressure profiles and leak point pressure determination, using a microtransducer catheter as the standard. METHODS: Ninety women without significant pelvic organ prolapse underwent urodynamic evaluations with both fiberoptic and microtransducer catheters. Maximal urethral closure pressures and “leak point pressures” were repeatedly measured by the two catheters and statistically compared. The order of catheter use was randomized. RESULTS: Significantly lower mean maximal urethral closure pressures were recorded by the fiberoptic system than by the microtransducer system. The fiberoptic catheter predicted microtransducer values for maximum urethral closure pressure only within a range of 27 cmH2O. Mean “leak point pressure” recorded by the fiberoptic catheters was not significantly different than that recorded by the microtransducer catheters. CONCLUSION: There is a significant difference between maximum urethral closure pressure values recorded by the microtransducer and fiberoptic catheter systems. No significant difference was found between the two systems in measurement of Valsalva “leak point pressure.”
Evaluation and treatment of female urinary incontinence
Abstract: With the aging of the female population and a new openness about urogynecologic health, Ob/Gyns are beginning to appreciate that urinary incontinence is a common problem in women. Here, 3 experts discuss the prevalence and economic impact of incontinence in America, as well as the basics of office and urodynamic assessment and therapeutic options.
Abstract: With the aging of the female population and a new openness about urogynecologic health, Ob/Gyns are beginning to appreciate that urinary incontinence is a common problem in women. Here, 3 experts discuss the prevalence and economic impact of incontinence in America, as well as the basics of office and urodynamic assessment and therapeutic options.
Abstract: The aim of this study was to determine the characteristics of women who meet the criteria for intrinsic sphincteric deficiency (ISD) on maximum urethral closure pressure (MUCP) but not on leak point pressure (LPP) measurement. We performed a cross sectional chart review of every patient who underwent multichannel, microtransducer urodynamic testing in our center between 1994 and 1996 (n=423). From this population we culled a sub-population of women who fit into one of the following two groups: women with no evidence of ISD on MUCP or LPP and women with evidence of ISD on MUCP only. Logistic regression was used to identify independent predictors of group membership. Increasing age (>60.5 years) and a positive supine empty stress test were the only independent predictors of membership in the group of women with ISD on MUCP only. Knowledge of these risk factors may help clinicians in choosing appropriate pre-operative testing.
Urethral retro-resistance…a new urodynamic measurement
Abstract: The urethral retro-resistance pressure (URP) is a retrograde urethral pressure profile measured by a new urodynamic measurement system. URP is the pressure required to achieve and maintain an open sphincter. This clinical investigation focused on a comparison of URP to standard urodynamic measurements and an examination of their relationship to incontinence severity. Methods: Twenty-two centers enrolled 258 stress incontinent women in a randomized, crossover study of two groups: (1) test procedure followed by multichannel urodynamics, (2) multichannel urodynamics followed by test procedure. We defined incontinence severity categories using 24 hr urine loss and assessed these categories using incontinence quality of life (I-QOL), urinary incontinence severity score (UISS), incontinence visual analogue score (VAS), URP, maximum urethral closure pressure (MUCP), and leak point pressure (LPP). Results: The mean age was 56.2 years. No order effect was present. The correlation coefficient between URP and MUCP was 0.31; between URP and LPP was 0.28; and between MUCP and LPP was 0.14. The mean values for URP across symptom severity categories were significantly different and decreased with increasing severity. The mean values for MUCP and LPP did not decrease with increasing severity. Conclusions: The study demonstrated that URP had a consistent relationship with incontinence severity. The data suggested that URP is a physiological measure of urethral function and may have clinical utility as a diagnostic tool. Future outcomes-based research is necessary to establish the predictive value of URP, MUCP, and LPP measurements in terms of incontinence cure rates and diagnosis of sphincter dysfunction.
Comparison of microtransducer and fiber optic urodynamic catheters
Abstract: OBJECTIVE: To assess the validity and reproducibility of a fiberoptic transducer urodynamic catheter for urethral closure pressure profiles and leak point pressure determination, using a microtransducer catheter as the standard. METHODS: Ninety women without significant pelvic organ prolapse underwent urodynamic evaluations with both fiberoptic and microtransducer catheters. Maximal urethral closure pressures and “leak point pressures” were repeatedly measured by the two catheters and statistically compared. The order of catheter use was randomized. RESULTS: Significantly lower mean maximal urethral closure pressures were recorded by the fiberoptic system than by the microtransducer system. The fiberoptic catheter predicted microtransducer values for maximum urethral closure pressure only within a range of 27 cmH2O. Mean “leak point pressure” recorded by the fiberoptic catheters was not significantly different than that recorded by the microtransducer catheters. CONCLUSION: There is a significant difference between maximum urethral closure pressure values recorded by the microtransducer and fiberoptic catheter systems. No significant difference was found between the two systems in measurement of Valsalva “leak point pressure.”
Can Urethral Retroresistance Pressures Predict Midurethral Sling Outcomes
Objective: To determine whether preoperative urethral resistance pressure (URP) measurements could predict success or failure of a tension-free vaginal tape (TVT) sling. Methods: Subjects came from a previously published study comparing URP measurements to a validated urinary incontinence system survey (UISS). We contacted patients from that study to determine whether they had subsequently undergone TVT surgery. Within that cohort, we determined the “current” (i.e., postoperative) UISS and Sandvik urinary incontinence severity score. Success of a TVT sling in this group was defined in 4 ways: (1) postoperative UISS score < 3, (2) postoperative UISS score < 75% of the preoperative score, (3) postoperative Sandvik score < 6, and (4) postoperative Sandvik score < 2. These definitions of “success” were compared across demographic and treatment variables. Results: We contacted 69 women who had in fact received a TVT sling after their participation in the previously published study mentioned above. Among these 69 women, mean preoperative urethral retroresistance pressure values were not predictive of surgical success. Conclusion: Preoperative urethral retroresistance pressure measurements did not reliably predict surgical success or failure; therefore, this urodynamic test is of little value to the clinician.
Various Subjects
Predictive validity of a training protocol using a robotic surgery simulator
Abstract: Robotic surgery simulation may provide a way for surgeons to acquire specific robotic surgical skills without practicing on live patients. Five robotic surgery experts performed 10 simulator skills to the best of their ability and thus established expert benchmarks for all parameters of these skills. A group of credentialed gynecologic surgeons naïve to robotics practiced the simulator skills until they were able to perform each one as well as our experts. Within a week of doing so, they completed robotic pig lab training, after which they performed supracervical hysterectomies as their first-ever live human robotic surgery. Time, blood loss and blinded assessments of surgical skill were compared between the experts, novices and a group of control surgeons who had robotic privileges but no simulator exposure. Sample size estimates called for 11 robotic novices to achieve 90% power to detect a 1 SD difference between operative times of experts and novices (α = 0.05). 14 novice surgeons completed the study – spending an average of 20 hours (range 9.7 to 38.2) in the simulation lab in order to pass the expert protocol. The mean operative times for the expert and novices were 20.2 min and 21.7 min, respectively (p=0.12),whereas the mean time for control surgeons was 30.9 min (p<0.0001). Comparisons of EBL and blinded video assessment of skill yielded similar results. Completing this protocol of robotic simulator skills translated to expert-level performance of live human surgery. As such, we have established predictive validity of this protocol.
Pilates to strengthen the pelvic floor
Abstract: The purpose of this study is to determine whether a Pilates exercise program and a pelvic floor muscle-training (PFMT) program could provide similar improvements in pelvic muscle strength. Methods: Sixty-two women with little or no pelvic floor dysfunction were randomized to Pilates or PFMT. Each group had 24 biweekly 1-h sessions with either a physical therapist or Pilates instructor. Strength was measured via perineometry (cmH2O). Two questionnaires—pelvic floor distress inventory and pelvic floor impact questionnaire were also collected. Both the Pilates and PFMT groups got stronger with no difference between groups. Conclusions: While the Pilates program can clearly result in stronger pelvic floor muscles, further study is required to determine if Pilates can actually treat pelvic floor dysfunction.
Bacterial colony counts during vaginal surgery
Abstract: Objective: To describe the bacterial types and colony counts present before and during vaginal surgery. Methods: A descriptive study was undertaken of patients undergoing vaginal hysterectomy with or without reconstructive pelvic surgery. Aerobic and anaerobic bacterial cultures were obtained immediately before and throughout the surgical cases at preselected time intervals. Standard antimicrobial prophylaxis was administered in all cases. Mean total colony counts and mean anaerobic colony counts were determined by adding all colonies regardless of bacteria type. ‘Contamination’ was defined as >= 5000 colony-forming units/ml. Results: A total of 31 patients aged 26 to 82 years were included. The highest total and anaerobic colony counts were found at the first intraoperative time interval. On the first set of cultures (30 minutes after the surgical scrub), 52% of the surgical fields were contaminated, and at 90 minutes, 41% were contaminated. A negligible number of subsequent cultures were contaminated. Conclusions: Any future interventions designed to minimize bacterial colony counts should focus on the first 30 to 90 minutes of surgery, because that is the time during which the operative field is the “dirtiest”.
4 steps to evaluation of asymptomatic microscopic hematuria
(Contemporary OB/GYN)Abstract: Microscopic hematuria is common and can be caused by a wide variety of medical conditions. The strict definition of hematuria is three or more red blood cells (RBCs) per high-power field in at least two of three properly collected urinalysis specimens. But there is no threshold of microscopic hematuria under which significant disease can be ruled out. In this article, I lay out a four-point plan for evaluating women with asymptomatic microscopic hematuria, based on the latest data in the medical literature.
A comparison of vaginal and laparoscopic suture placement through the uterosacral ligaments
Abstract: OBJECTIVE: To compare the tensile strength of two approaches for uterosacral ligament suturing using a cadaver model. METHODS: In 12 unembalmed cadavers, four polytetrafluoroethylene sutures were placed through the uterosacral ligaments. In each cadaver, two sutures were placed laparoscopically, and two more were placed vaginally. A single, experienced surgeon placed all laparoscopic sutures, and another experienced surgeon placed all vaginal sutures. A blinded team of investigators measured the distance from each suture to the ipsilateral ischial spine; determined whether any sutures incorporated ureters, viscera, or large vessels; and then passed the sutures through an apical vaginal incision. Using a hand-held tensiometer, progressive tensile load was then applied to these sutures along the axis of the vagina until they either broke or were completely dislodged from the ligaments. CONCLUSION: These suturing techniques appear to be equal in terms of tensile strength.
Anti-sperm antibody testing before IVF
Abstract: Objective: To determine the usefulness of and cost-effectiveness of antisperm antibody testing in the prediction of poor fertilization rates in couples undergoing IVF. Design: Retrospective cohort study. Setting: A hospital-based reproductive endocrinology and infertility practice. Patient(s): Male partners of 251 couples undergoing IVF between 1992 and 1997. Main Outcome Measure(s): Fertilization rates in couples undergoing conventional IVF. Result(s): One hundred nineteen couples were evaluated for antisperm antibodies; fertilization rates were similar in those couples whose husbands were and were not tested (64% versus 68%). Antisperm antibodies were detected in 16 men. Four (25%) of the 16 couples whose husbands had antisperm antibodies fertilized #50% of oocytes, compared with 31 (30%) of the 103 couples whose husbands did not have these antibodies. Overall, 21 couples (8.4%) experienced complete fertilization failure. In a program that included antisperm antibody testing for selected couples and intracytoplasmic sperm injection (ICSI) for those who tested positive, it would cost $11,735 to prevent a fertilization failure (assuming ICSI were 100% effective), whereas it would cost $9,250 to perform ICSI in a second IVF cycle for those who initially failed. Conclusion(s): In this practice setting, antisperm antibody testing has low sensitivity in predicting low or no fertilization and does not appear to be cost-effective when selectively ordered as part of an IVF workup.
Effects of childbirth on the pelvic floor
Abstract: The majority of childbirth injuries to the pelvic floor occur after the first vaginal delivery. Cesarean sections performed after the onset of labor may not protect the pelvic floor. Elective cesarean section is the only true primary prevention strategy for childbirth injuries to the pelvic floor. Alternative primary prevention strategies include elective cesarean section for women with nonmodifiable risks for childbirth injuries to the pelvic floor, antepartum pelvic floor exercises, or intrapartum pudendal nerve monitoring. Secondary prevention strategies must focus on modifying obstetric practices that predispose women to pelvic floor injury. These factors are best delineated for anal incontinence and include restrictive use of episiotomy, mediolateral episiotomy when necessary, spontaneous over forceps-assisted vaginal delivery, vacuum extraction over forceps delivery, and antepartum perineal massage. Finally, tertiary prevention strategies should address the mode of delivery made for women with childbirth injuries to the pelvic floor who desire future fertility.
Pubic symphsis separation during childbirth
Abstract: BACKGROUND: Rupture of the symphysis pubis during vaginal delivery is a rare but debilitating complication. Factors contributing to rupture are poorly defined. CASE: A healthy primigravida suffered a rupture of her symphysis pubis during an otherwise uncomplicated vaginal delivery. She experienced significant pain and difficulty walking for 6 months after the injury. Her 5-cm symphyseal separation was managed successfully with physical therapy and activity restriction. The patient’s two subsequent deliveries (one vaginal and one via cesarean delivery) were uneventful. CONCLUSION: Severe symphyseal rupture during vaginal delivery can be managed without surgery. Risk factors for rupture are not well defined. Based on a literature review, there is a significant risk of repeat symphyseal rupture with subsequent vaginal delivery.
Decision Analysis regarding Elective C-section and Macrosomia
Abstract: Our aim was to determine the cost-effectiveness of a policy of elective C-section for macrosomic infants to prevent maternal anal incontinence, urinary incontinence, and newborn brachial plexus injuries. We used a decision analytic model to compare the standard of care with a policy whereby all primigravid patients in the United States would undergo an ultrasound at 39 weeks gestation, followed by an elective C-section for any fetus estimated at ‡4500 g. The following clinical consequences were considered crucial to the analysis: brachial plexus injury to the newborn; maternal anal and urinary incontinence; emergency hysterectomy; hemorrhage requiring blood transfusion; and maternal mortality. Our outcome measures included (1) number of brachial plexus injuries or cases of incontinence averted, (2) incremental monetary cost per 100,000 deliveries, (3) expected quality of life of the mother and her child, and (4) ”quality-adjusted life years” associated with the two policies. For every 100,000 deliveries, the policy of elective C-section resulted in 16.6 fewer permanent brachial plexus injuries, 185.7 fewer cases of anal incontinence, and cost savings of $3,211,000. Therefore, this policy would prevent one case of anal incontinence for every 539 elective C-sections performed. The expected quality of life associated with the elective C-section policy was also greater. A policy whereby primigravid patients in the United States have a 39 week ultrasound-estimated fetal weight followed by C-section for any fetuses ‡4500 g appears cost effective. However, the monetary costs in our analysis were sensitive to the probability estimates of urinary incontinence following C-section and vaginal delivery and the cost estimates for urinary incontinence, vaginal delivery, and C-section.
Randomized trial of two surgical scrubs for vaginal hysterectomy
Abstract: Objective: The purpose of this study was to compare the efficacy of chlorhexidine and povidone iodine for cleansing the operative field for vaginal surgery. Study design: This was a randomized controlled trial that compared 10% povidone iodine and 4% aqueous chlorhexidine gluconate as surgical scrubs. Our primary end point was the proportion of contaminated specimens per group found throughout the surgical procedures. All patients received standard infection prophylaxis that included preoperative intravenous antibiotics. Immediately before antibiotic administration and baseline aerobic and anaerobic cultures of the vaginal flora were obtained, which were followed by cultures at 30 minutes after the surgical scrub and hourly thereafter throughout each patient’s surgery. Results: A total of 50 patients were enrolled between October 2002 and September 2003. There were no differences between the povidone iodine and chlorhexidine groups with respect to age, race, exogenous hormone use, body mass index, gravity, parity, preoperative mean colony counts, or operative time. Among the first set of intraoperative specimens (which were obtained 30 minutes after the surgical scrub), 63% of the cultures from the povidone iodine group and 22% of the cultures from the chlorhexidine group were classified as contaminated. Subsequent cultures failed to demonstrate significant differences. Conclusion: Chlorhexidine gluconate was more effective than povidone iodine in decreasing the bacterial colony counts that were found in the operative field for vaginal hysterectomy.
Abstract: Objective: The purpose of this study was to determine the effects of extracorporeal magnetic innervation (ExMI) on pelvic muscle strength of primiparous patients. Study design: Primigravid patients were randomized to receive either active or sham ExMI postpartum treatments for 8 weeks. The main outcome measure was pelvic muscle strength measured by perineometry at baseline (midtrimester), 6 weeks (before treatments), 14 weeks, 6 months, and 12 months postpartum. Mixed randomized-repeated measures ANOVA was used to analyze the mean perineometry values between the 2 groups and across all 5 time periods. Results: Fifty-one patients enrolled, and 18 were lost to attrition. There were no differences in demographics or delivery characteristics between the active and sham groups. There was an overall time effect, but no group, or (group)(time) interaction. Conclusion: We found no differences in pelvic muscle strength between patients receiving active or sham ExMI treatments in the early postpartum period. Therefore we believe that Neotnous treatments given after vaginal delivery will not benefit new mothers.